Quick Read:
- Early surges of influenza and RSV continue to strain emergency departments and spark public-health concerns.
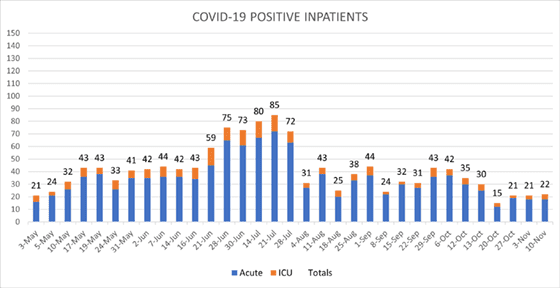
- Newer omicron subvariants are now responsible for more than half of all COVID-19 infections in the U.S., but local COVID-19 activity remains low.
- UW Medicine has discontinued use of the antibody treatments Evusheld and bebtelovimab as neither therapeutic has proven effective against newer omicron strains.
- Tomorrow is the deadline for meeting UW Medicine’s COVID-19 bivalent booster campaign requirement.
The early arrival of influenza and other respiratory viruses this fall continues to pose major challenges to health systems nationwide, including UW Medicine. While we have not yet seen a similar spike with COVID-19, newer omicron subvariants are accounting for an ever-larger share of infections as the virus evolves and mutates.
Our teams are closely monitoring these trends, some of which are having an outsized impact on our local hospitals and clinics. In particular, we continue to see cases of respiratory syncytial virus (RSV) driving visits to emergency departments locally and across the country. RSV cases began rising in early September and have grown exponentially in recent weeks, placing an enormous strain on emergency department, urgent care and primary care clinic staff. Although most of these patients are children, older adults and immunocompromised people also are especially vulnerable.
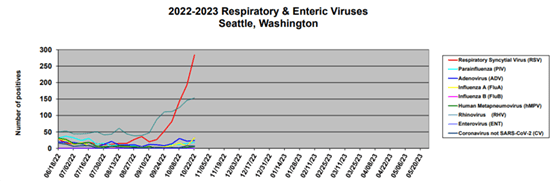
Local cases of respiratory syncytial virus (RSV) began spiking in early September, much earlier and far faster than in previous years. (Source: UW Virology)
In many parts of the country, we’re also seeing an uncommon number of influenza and influenza-like infections for this time of year. The Southeast, for example, is seeing a huge spike in flu-like illness, with levels of activity that haven’t been seen this early in the season for more than a decade. Regional outbreaks often spread to other parts of the country, so we should take this as a warning and prepare to see more influenza in our region and community in the weeks ahead.
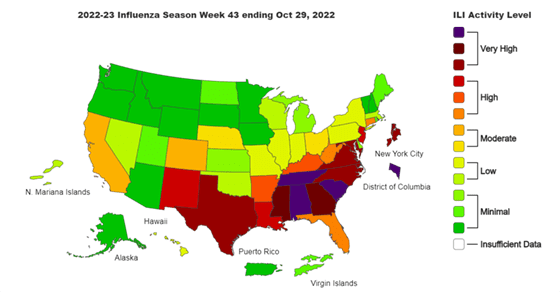
The flu season has arrived earlier than usual. Right now, it’s impacting the southern U.S. hardest, but we should be prepared for local spikes in the weeks ahead. (Source: CDC)
Meanwhile, COVID-19 remains a serious threat to public health entering the winter months. According to data from the Centers for Disease Control and Prevention (CDC), a handful of newer omicron subvariants now account for more than half of all infections nationwide. That includes the BQ.1 and BQ.1.1 subvariants, which now are responsible for more than 35% of all COVID-19 infections nationally — more than twice the number from two weeks ago. This subvariant “soup” has displaced the BA.5 variant that as recently as late August was causing more than 86% of U.S. infections.
Unfortunately, the changing nature of the virus is rendering some of our most impactful COVID-19 therapeutics ineffective. This week, we discontinued our use of Evusheld and bebtelovimab. Both of those antibody treatments worked well against earlier strains of the virus but have proven much less effective against the newer omicron subvariants. The good news is that the oral antivirals appear to maintain their activity. We are also operationalizing use of remdesivir, an intravenous antiviral, for use in patients with COVID-19 infection who are immunocompromised and cannot receive oral antivirals. Our best advice for individuals who are immunocompromised continues to be that they stay current on their boosters and follow best practices for masking and physical distancing.
Final Reminder to Get Boosted
Tomorrow is the final day of our bivalent booster campaign. All UW Medicine employees, except for those in non-clinical roles in the School of Medicine, are required to participate by either getting the new COVID-19 bivalent booster or completing the online declination.
If you haven’t already received the new booster, I strongly encourage you to make an appointment today. It’s a decision that could save your life or the life of somebody you love. You can schedule through our online portal at c19-vaccine.uwmedicine.org.
Non-clinical employees in the School of Medicine, and all other University of Washington employees, students and contractors, should call 844.520.8700.
UW Medicine COVID-19 Activity Summary
Local/National/Global Epidemiology
King County: Public Health – Seattle & King County is reporting 525,736 total cases and 3,266 deaths as of Thursday, Nov. 10. The number of new positive tests over the past seven days is currently at 48.6 per 100,000 people.
Washington: The Department of Health reports 1,843,908 cases and 14,653 deaths as of Nov. 8.
United States: The Centers for Disease Control and Prevention reports 273,110 new cases weekly, 97,604,763 total cases and 1,068,667 deaths as of Nov. 9.
Global: The WHO COVID-19 Dashboard reports 630,601,291 confirmed cases and 6,583,588 deaths as of Nov. 10.
Harborview COVID-19 Test Site
Two weeks ago, we noted the closing of our COVID-19 test site at UW Medical Center – Northwest and its historical significance as the first drive-through COVID-19 testing location in the country. I want to acknowledge in a similar way our test site at Harborview, which was transitioned this week to our Laboratory Medicine team. This site grew out of the emergent need to provide rapid access to testing healthcare workers, first in a conference room at Harborview, then a tent in front of the hospital, and finally a building where thousands of people have since been tested.
These test sites, along with others in our system, were at the heart of our COVID-19 response through the most difficult days of the pandemic. I will always be grateful for the sacrifices and commitment of our leaders and colleagues who formed them and showed up every day to protect our community and serve our mission.
To those who continue working at our other test locations around the region and to everybody who continues to be involved in our ongoing response to COVID-19, I also say thank you. Your work matters and is making a difference.
One more note of gratitude is for all the veterans in our community and especially those whom we are fortunate enough to call colleagues in UW Medicine. Thank you for your willingness to serve and sacrifice for our country. Happy Veterans Day!
Sincerely,
John Lynch, MD, MPH
Medical Director, Infection Prevention & Control
Associate Medical Director, Harborview Medical Center
Division of Allergy & Infectious Diseases, UW School of Medicine
