Highlights | Robot-assisted surgery
- Robotic surgeries are minimally invasive with less patient downtime, and they are more ergonomic for surgeons.
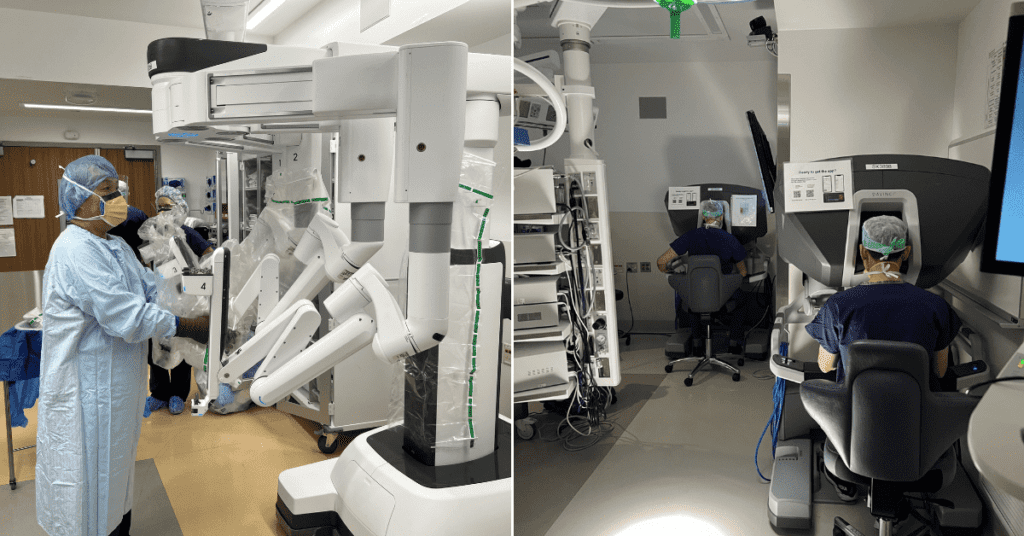
- The robot consists of a surgeon console, robotic arms (patient cart) and a camera connected to the central processing unit (vision cart).
- The robot arms mimic the surgeon’s movements in the surgeon console.
- Eight specialties at UW Medicine utilize robots for their surgeries.
During his fellowship training, James (Jim) Park, MD, FACS, vowed he would never do robotic surgery when he “grew up” (aka completed his fellowship). Now, 70% of his cases are robotic surgeries. He became the first person in the Pacific Northwest to do a robotic liver resection and the first person in Washington state to do the robot-assisted Whipple procedure. He’s also co-chair of the Robotic Steering Committee, clinical director of Surgical Specialties for the WWAMI Institute for Simulation in Healthcare (WISH) and director of the UW Liver Tumor Clinic.
Park’s initial dislike for robotic surgery stemmed from a negative exposure to robots during his training when the technology was relatively brand new; now, he’s invested in teaching his trainees so they can bring these less invasive surgical tools to their future patients and move the field forward.
What is robotic surgery?
Robotic surgery utilizes a fiberoptic camera inserted into the abdomen (laparoscopic), chest (thoracoscopic) or mouth (trans-oral) for visualization, and the surgeon controls two or three robotic instruments to perform surgeries as a minimally invasive approach instead of open surgery.
Preparing for surgery.
“The robot used in surgical practice, at least in 2022, is a non-autonomous unit with no artificial intelligence, i.e., does not have a mind of its own,” says Park. “The robot mimics and reproduces everything the surgeon does.”
Like pure laparoscopic surgeries, robotic surgeries that Park performs require five small incisions: one for the camera, three for the instruments and an additional incision for an assistant. The major difference is that with robotic surgeries, the surgeon works from a surgeon console, where they use the master controls to tell the robot what to do.
“Despite my experience in fellowship, I saw there were benefits to patients in terms of having less trauma inflicted on them, which results in less pain and earlier recovery — not only leaving the hospital sooner but returning to life and going back to work or doing the things they love faster,” says Park.
There are also added benefits with robotic surgery for the surgeon: they get a clear 3D view that provides depth perception; it’s ergonomically advantageous, especially for those six-to-eight-hour surgeries; and it has wristed instruments that allow for more complex movements. It also removes tremors, which Park says he thankfully does not need yet.
“I see the robot as an extension of my hands,” says Park. “But the relationship I have with this tool is a little more than what I have with a scalpel or the regular open or laparoscopic tools, as it does enhance my visualization and tissue handling.”
The downside is that the current commercial surgical robot lacks haptic feedback. Haptic feedback is the sensation you can feel with your hands, like the instruments hitting up against fragile tissue, explains Park. In robotic surgery, you don’t get the same tactile feedback as with open or pure laparoscopic surgery, so you must develop a visual sense of haptics. It’s a skill you have to learn and one that he teaches his students.
“As you gain more experience, your brain fools you into thinking that you have haptics in your hands,” says Park. “When I train my residents, I keep telling them to feel with their eyes.”
Historic firsts
With robotic technology, Park has completed pioneering surgeries, robot-assisted Whipple procedure (2012) and the first robotic liver resection (2011) that have paved the way for other surgeons in the Pacific Northwest.
He isn’t the only surgeon at UW Medicine to have completed historic firsts in robotic surgery.
In 2010, Barbara Goff, MD, performed the first robotic hysterectomy in Washington state, William Ellis, MD, completed the first robotic prostate surgery procedure in Washington and Eduardo Mendez, MD, performed the first trans-oral robotic surgery in Washington.
“When you are the first it’s exciting, but you have to be cautious not to mess it up for everyone else,” says Park.
Robotic surgery is relatively new — the first iteration of robots was Food and Drug Administration (FDA) approved in 2000 — and UW Medicine was an early adopter of the technology, investing in a robot in 2003 and completing three procedures that year.
Now, we have eight subspecialties performing approximately 2000 robotic cases annually, with urology, gynecology and general surgery being the most frequent users.
Robot Olympics
Other frequent users are Park’s residents, the surgeons of tomorrow, who assist in cases and use a credentialling backpack simulator as part of their training.
“Many academic institutions have been allotted these simulators, and we are the highest volume user nationally. This is a testament to our residents’ dedication to their training, and our faculty’s commitment to the educational mission,” says Park.

Residents training using the robotic surgical equipment.
To keep the unit that the manufacturing company distributes, they must prove that they use it (because, as you can guess, this technology is expensive). One way Park does this is, in his words, “we capitalize on the competitive nature of resident surgeons with the Robotic Simulation Olympics.”
The backpack console has games that simulate surgical techniques. The system scores and provides feedback on how well the surgeon did. We change up the themes of these competitions to keep it fresh and exciting, from the Winter Olympics to March Madness, to Fanta-SIM Football.

Residents training using the robotic surgical equipment.
Beyond the Olympics, the backpack console is also used for certification or recertification. For a resident to be able to assist in an OR case they must complete five games in the 90th percentile — so beyond being fun, it’s crucial for training and maintenance of skills.
Park even uses the simulator to warm up by completing simulation modules before some of his surgeries.
The future of robotic surgery
As Park looks toward the future of robotic surgery, his focus is on resident training and advancing technology.
“My job as an academic robotic surgeon is to make sure that my residents and future surgeons have a better experience than I had when I was in training. Also, I believe that surgeons need to be involved in developing new technology and guiding its implementation.”
Park is hoping to grow the training program and advance the technology. Park and his colleagues developed a dedicated training curriculum for their residents, and he has a collaboration with the robotic industry scientists to develop technology that will overlay 3D renderings of preoperative imaging into the surgeon’s console viewer for real-time navigation. He’s also excited for manufacturing companies to improve upon the current single port technology with flexible camera and instrument arms working through one incision instead of four.
“I’m hoping we can develop a robot with six or eight arms — like Dr. Octavius in Spiderman,” he says.
Beyond the octopus-like arms, what really makes robotic surgeries successful is the team.

Park (far right) and his surgical team.
“From the surgeon to the nursing staff, scrub tech team and anesthesiologists, it takes everyone’s expertise to have a successful operation,” says Park. “I am lucky to be part of the UW Medicine team where everyone goes above and beyond for the patient.”