Highlights | Preparing for worst-case scenarios
- Every year, Harborview Medical Center conducts an annual patient decontamination drill.
- The drill prepares for a scenario where patients need to be decontaminated from exposure to a hazardous material before entering the hospital.
- Staff practice properly donning and doffing personal protective equipment and learn protocols.
- Practicing helps inform and improve the procedures we already have in place.
As a Level 1 Trauma Center, Harborview Medical Center is always preparing for worst-case scenarios.
Every year, Harborview conducts its annual patient decontamination drill.
The scenario they are practicing for: A massive industrial incident or other situation involving hazardous materials.
In the event of a mass casualty incident where patients need to be washed off in masses to protect the hospital from exposure to hazardous material, like chemical, biological or radioactive materials, Harborview teams need to know what to do.
Mark Taylor, BSN, RN, CCRN-K, interim associate administrator at Harborview, says that although this scenario is logistically unlikely, it’s good to be prepared.
“In most mass biohazard events, the patients that would be brought to us would have already been decontaminated at the scene,” says Taylor. “This scenario is if there was a chemical spill in the neighborhood and a large number of patients, maybe 15-20, walked to the hospital with symptoms like itchy or watery eyes and skin irritation.”
Harborview does have the ability to decontaminate small numbers of people in the Emergency Department’s decontamination room (which Taylor notes is used more frequently than you might expect) but for scenarios with larger groups of people needing decontamination, they have outdoor decontamination tents to do the job.
Deploying the Patient Decontamination Team
The Emergency Department (ED) nurse attending and charge nurse run the show. If they were to receive a call that a large number of people were coming in with possible exposure to a biohazard, they would be the ones to activate the mass decontamination process.
On the clinical side, one to two staff members from each of the inpatient units would report to the ED to be part of the decontamination team. This leaves ED staff available to take care of incoming patients.
Engineers on-site would also deploy to set up the decontamination tents and traffic control and security would block off the designated decontamination area on Jefferson Avenue.
Practice makes prepared
The drill starts with the assembly of the decontamination tents that are used to shower off patients who may have come in contact with hazardous materials.
“There is one side of the tent that patients go through on a stretcher and one side for patients that can walk through,” says Taylor.
The tent acts a bit like a wading pool, with the runoff water draining into containment bladders that get disposed of by hazmat crews to prevent chemicals from draining into the Puget Sound.

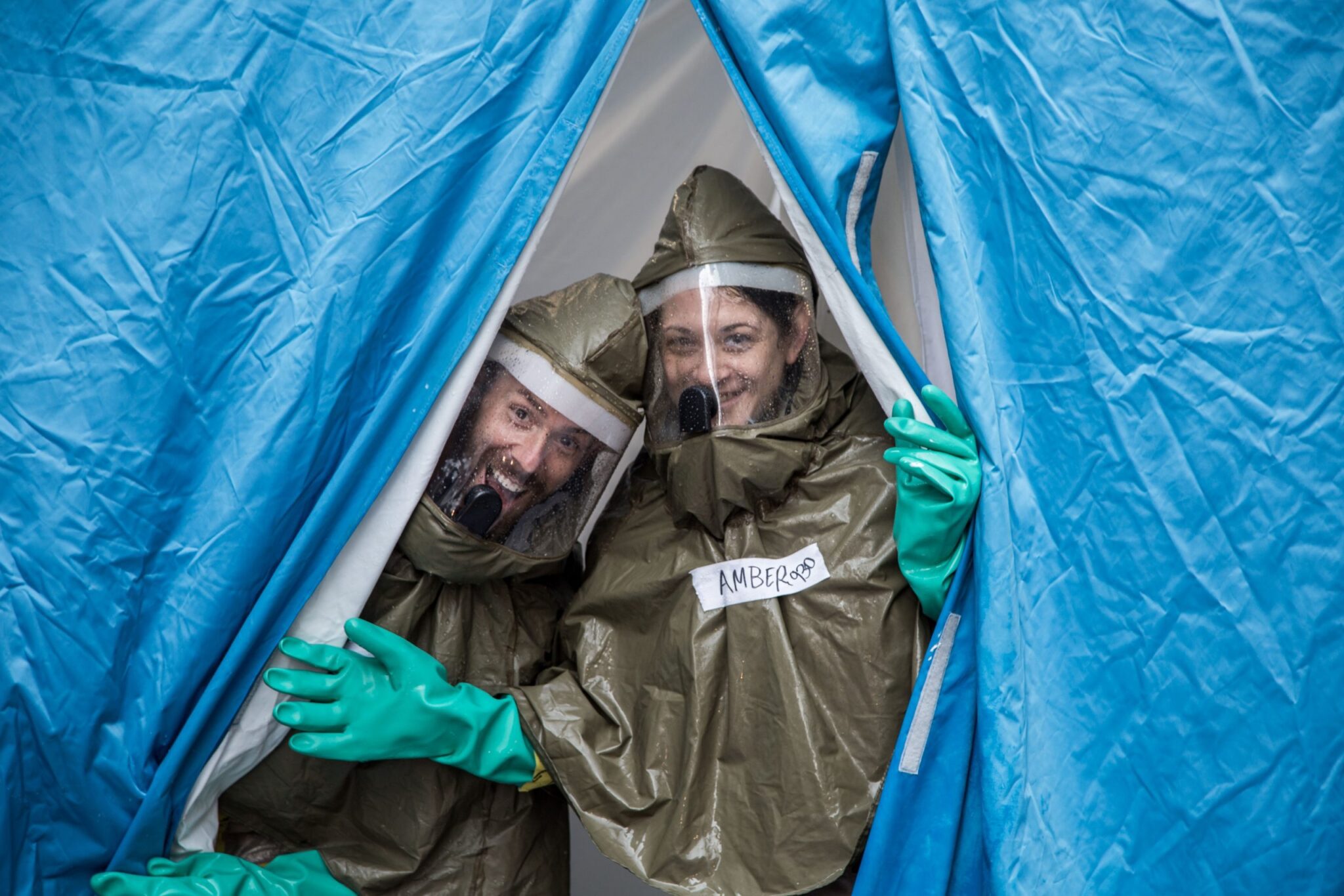
Staff in PPE enter decontamination tent for the drill.
One of the most important aspects of the training is learning to don and doff (take on and off) PPE.
“We want to make sure our staff, the people who are healthy, stay healthy so we don’t create more patients,” says Taylor.
That’s where having practice with PPE comes in. The clinical staff use Level C PPE, which includes a chemical-impermeable suit and a powered air purifying respirator (PAPR) that protect against a variety of chemicals and biological agents.
“It’s similar to what our staff have used during COVID-19, but this is a higher level of PPE,” says Taylor. “It’s physically bulkier, more restrictive and larger.”

Staff wearing Level C PPE.
Once staff are geared up, they bring in the “patients,” which this year, due to COVID-19 restrictions, is just a board. As the patients, or boards, go through the tents for decontamination, they are hosed down by the clinical staff in their PPE.
Taylor says that in previous years, they have had volunteers come in to act as the patients. The volunteer “patients” were covered in shaving cream (to simulate the biohazard material) so the decontamination team had a visual of how well the process was working and where they needed to make improvements.
“We do heat the water, so it’s not straight out of the fire hydrant,” says Taylor. “It’s really not a bad experience on a summer day.”

Staff hose down a board as part of the simulation training.
It’s all timed and observed. The training exercises and tents need to be completed or set up in a certain amount of time and the don and doff PPE procedures are closely observed to ensure protocols are followed.
Taylor says there is some room for fun too, though.
“We take it seriously because it’s a serious event, but it’s also summer and we are getting hosed down — it’s hard to not have a little bit of fun with that,” he says.
Staff in PPE in the decontamination tent.
Lessons learned
Taylor says the drill went smoothly and as planned, but there are always lessons to learn. The observation team is working on going through their notes and observations to make decisions on what needs to be updated.
It’s also an opportunity for staff to see what they already know and to gain confidence that they have the tools and knowledge to react should the simulation they’ve practiced for happen in real life.
“Harborview is in the business of being prepared,” says Taylor. “We take patients no matter how they present and drills like this allow us to do just that. Our staff are ready and comfortable with the equipment so we can operate safely and efficiently to get our patients care as soon as possible.”


