Okay, hold onto your face coverings … this well-being message is going to get into some of the challenges we are facing now and will look forward at what we can anticipate coming down the road over the months to come. Let’s jump in … before this pandemic, nearly half of physicians and nurses in the United States reported experiencing burnout, and we anticipate those numbers will increase as a result of the pandemic. An early study of the mental health of healthcare workers in Wuhan following COVID-19 found 72% of individuals in a sample exhibited at least one symptom of PTSD. While the well-being of healthcare workers was compromised before COVID-19, the increased urgency for support and intervention in the current environment transforms the present into a unique moment to address both emergent and entrenched long-term needs.
We can learn about COVID-19 response and recovery from previous research on disaster recovery. The trends in emotional responses to previous events indicate we are likely to navigate feelings of disillusionment and a slow road of emotional well-being recovery over the next one to three years. COVID-19 adds a layer of complexity to traditional disaster recovery models in that we have on-going uncertainty around the possibility of resurgences that would exacerbate financial issues, disrupt recovery and add a layer of stress to an already highly burdened population. Ready for the scary graph?
Typical emotional trajectory through a disaster for a population

Adapted from Zunin & Myers as cited in DeWolfe, D. J., 2000.
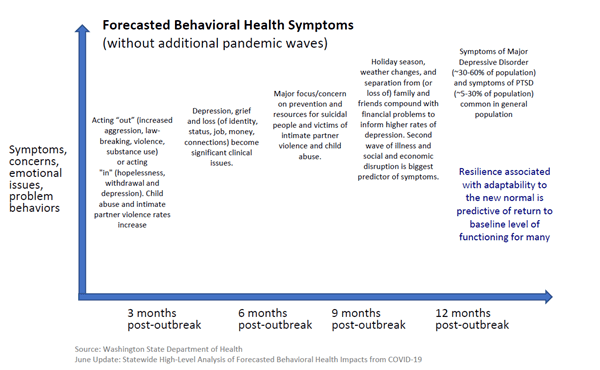
The Washington State Department of Health’s June report on forecasted behavioral health impacts of COVID-19 indicates that we will hit our peak health impacts 6 to 9 months after the initial outbreak, which corresponds to October through December in our area. Additional peaks and waves will exacerbate and prolong the health impacts on our community broadly and UW Medicine team members specifically. While Washington state is not currently predicting large spikes in PTSD given our successful avoidance of the first-wave surge we feared in the worst-case scenario, we are anticipating high levels of burnout and very high rates of depression due to chronic social and economic impacts (as opposed to the acute impacts in single event disasters). We also anticipate significant increases in self-medication over the next 6 to 9 months; looking at comparative sales from May 2019, marijuana purchasing is up 44% and alcohol sales are up 31% this year. The graph below shows anticipated symptoms and concerns in the months ahead.
Forecasted Behavioral Health Symptoms (Without Additional Pandemic waves)
While the trajectory of a typical behavioral response is sobering, the good news is that baseline resilience and acquired resilience coping skills during the crisis recovery can improve our response and the speed of returning to baseline.
What can we do now to mitigate the impacts of COVID-19?
- Focus on social connections even as we maintain physical distance.
- Leverage resilience coping skills. Get outside! Move your body! Eat well! Sleep!
- Normalize behavioral responses, validate emotions and destigmatize reactions.
- Prepare for changes in school and childcare schedules and potential closures.
- Know that the normal reaction to disasters is resilience. Leverage relationships, foster positive emotions and stay anchored in your sense of purpose.
Some of you will have looked at the scary graph and thought, “I actually feel pretty good …” while others will stare at it and think, “this explains a lot.” There is no prescribed path through COVID-19, but we do anticipate seeing friends, family, patients and even ourselves having challenging emotional responses now and in the months to come. As always, please take good care of yourself and the community around you. Leverage the resource of Peer Support and our Department of Psychiatry’s informal Supportive Conversations when you are facing challenging moments. Though there is still much uncertainty with COVID-19, I am more confident than ever in our ability to adapt and grow into an even stronger UW Medicine as we navigate the year ahead.
With gratitude,
Anne Browning, PhD
Assistant Dean for Well-Being, UW School of Medicine
Founding Director, UW Resilience Lab
Affiliate Assistant Professor, UW College of Education
Sources:
National Academies of Sciences, Engineering, and Medicine. (2019). Washington, DC: The National Academies Press.
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. (2020). JAMA Network Open. 3(3):e203976.

